We left off last week with the girls being whisked away to the NICU. For several reasons, such as my recovery and the NICU being shut to visitors because of an emergency, I didn’t see the girls again until they were 24 hours old. If I think about that too much my heart hurts a little. But, obviously, I’ve had two years and nine months so far to make up for that.
The girls were placed in the SCBU (special care baby unit), first in the high-dependency room and then the lower-dependency room. I remember walking in there for the first time and a nurse pointing at which incubators held my babies. They were at opposite ends of the room to each other which was strange, and a bit upsetting, since they had been so close internally.
The girls started off with breathing support, an IV, heart monitors on their chests, and a pulse monitor on their toes, so they were covered with wires and wearing tiny baby nappies that looked massive on them.


Bottom: Lily
I remember that the first time I went to visit the girls, I fainted outside the ward because I made the mistake of standing up for a bit too long just a day after having major abdominal surgery. Props to the receptionist who managed to catch me! Thankfully Sam was in with the girls so he was able to come out and make sure I was OK. Once I was back on the maternity ward I was in an awful amount of pain because my bladder was essentially frozen so they re-catheterised me and the relief was almost immediate. It meant that I had to walk down to the NICU with a bag of my wee strapped to my leg though.


It was very strange being up on the maternity ward with the girls down in the NICU. I was on a ward with a couple other NICU mums so there were no babies, which was a relief as I didn’t particularly want to be woken by other people’s babies, and I got to chat to them about our shared experience. I was torn between feeling exhausted and needing to recover from major surgery and desperately wanting to be with my babies. The midwives and health care assistants who were caring for me were gold standard, despite the crazy busyness of the ward. I’ll forever be grateful for the compassion and care they showed me in those first few days of recovery. One time I cried because I didn’t like the food on the menu and they kindly found me an alternative, like the diva I am.
Each day my recovery improved so that by 9th February (so 4 days after the girls were born), I was discharged home. Leaving the babies in the hospital and driving away was bizarre and heartbreaking, though we knew they were in the best hands. I returned each day thanks to my kind friends and Sam driving me there (as I couldn’t drive post C-section), so I didn’t leave them too long and Sam went to be with them every evening.
I didn’t first change Bethany and Lily’s nappies until they were a few days old and it took some guidance and maneuvering to avoid all the wires! Oftentimes I would let the nurses do those kinds of jobs so I could save my energy to focus on feeding and bonding with the girls. Initially, the girls were tube-fed using my colostrum which I managed to harvest (gross) when I was waiting for my C-section. Their tummies were only really tiny so they couldn’t manage much, and the IV was helping keep their fluids up. They also had vitamins through their IV drip each day, and other things that now I can’t remember. Eventually they would get my pumped breast milk through their tubes and were encouraged to suck on a dummy whilst that was happening so they connected the two sensations. Since the girls were fed using a syringe and tube, both Sam and I were able to feed them in the first few days, as well as the nurses.

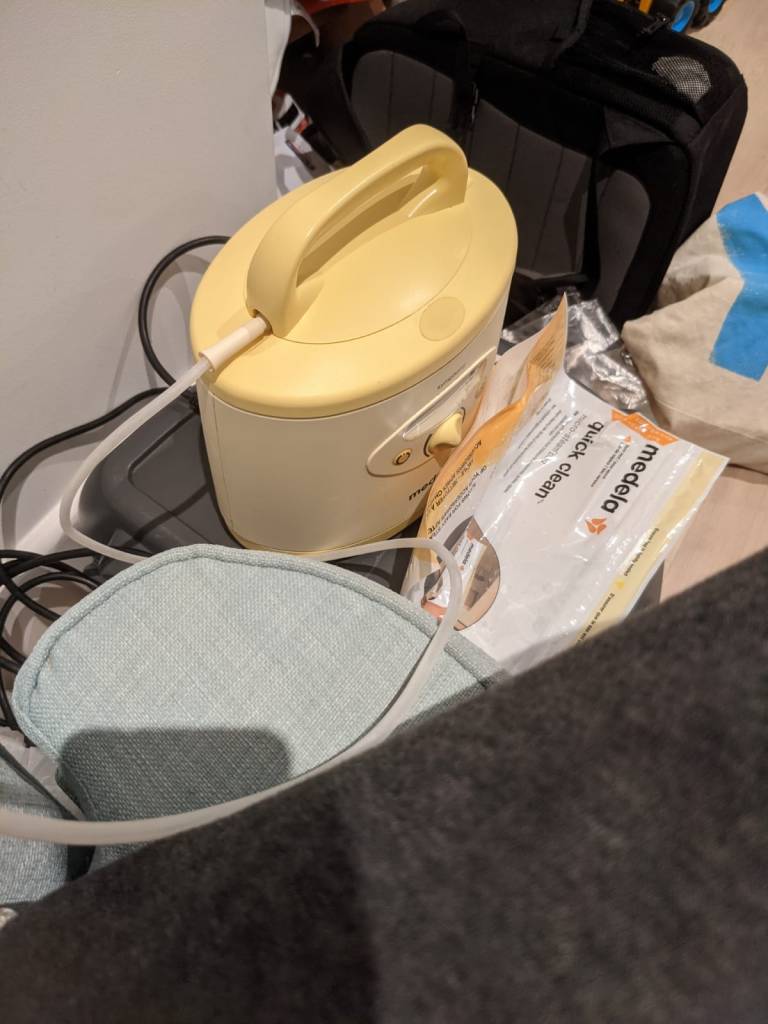
Ah, pumping. The least glamorous part of this process (not that anything was particularly glamorous, see bag of wee above). I was loaned a hospital-grade pump from the NICU which was amazing as I could take it home and it did make it easier and quicker. I had to pump at certain intervals during the day and set my alarm at night to pump once (much kinder than a newborn’s wake-ups!) I was fortunate to produce a crazy amount of milk which the NICU nurses often commented on as I stored it in their fridge. Each morning I would rock up with my cool bag full of milk to add to the fridge on the ward. There were so many processes of storing and labeling the milk, that I had totally forgotten until now. Like any difficult situation, you just get on with it and things that first seemed alien become second nature.
Before I was discharged home, I breastfed Bethany for the first time and she did really well. I’ll talk about the challenges of learning to breastfeed in the NICU a little later. When I was discharged, the girls were 4 days old. Lily was still on breathing support so I wasn’t able to feed her and they were both under treatment for jaundice (under a blue light). Bethany had been weaned off her fluids from the IV and they were hoping to do the same with Lily too. But they were both in individual incubators in the high-dependency room. So they still needed a decent amount of support.
The next few days saw the girls being weaned off breathing support and the liquids through their IVs as well as having their heart monitors removed. So gradually they were less encumbered by wires.

Each day I would try to put them to the breast to feed, though because they were so tiny and born so early (at 34 weeks), they were often too sleepy to feed. Credit must go to the incredible NICU nurses who helped me position them and myself so I could comfortably feed them with their teeny tiny mouths! I don’t think our breastfeeding journey would have been anywhere near as successful as it has been without the support of those nurses. I personally think every new mother should have days of breastfeeding support whilst in the hospital. I had so many challenges breastfeeding Caleb because no one came around whilst I was on the ward to show me how to do it. Thankfully I had the wonderful organisation BABIES in Winchester who supported me so well at home. The challenges with the girls were many: sleepy babies, tiny bodies and mouths, being in a strange environment, my boobs being too large (!) But we kept trying again and again. I was often limited in the length of time I could keep them out of their incubators, especially when they were under phototherapy for jaundice, so I was not able to have the amount of practice a new mother normally has with her baby. And there were two of them!!
Lily struggled a lot in the NICU with tolerating her feeds and consequently lost a lot of weight, going down to 4lbs. She also occasionally seemed to have heart problems so had a few ECGs and numerous blood tests. I’m so thankful for the wonderful doctors and nurses in the NICU who reassured us, kept us informed, and cared for the girls so well. There were plenty of other babies on the ward who needed a lot of support. One baby was born at 30 weeks and was so tiny, then there were several sets of triplets born in the few days after the girls were born! It was an incredibly busy ward. There were also the higher dependency intensive care wards which cared for the very ill babies. Whilst we never saw those babies, my heart was with them and their parents each time an emergency alarm sounded that led doctors to go rushing into the room.
When the girls were just over a week old, they were moved to the lower dependency room of the SCBU and put in a cot together!

As you can see in the photo, they were fully wire-free apart from the pulse monitor on their toes and their feeding tubes. It made taking them out for cuddles and feeds so much easier! It also meant Sam and I could hold them both at the same time which was a joy!

Occasionally the girls needed to receive phototherapy for jaundice again so they would both be squeezed into the same incubator for that. They were regularly weighed, and orally given vitamins and I would practice feeding them daily.
Whilst we were initially told the girls would be in for at least 2 weeks, we were obviously hoping it would be for less time than that. However, their stay in the hospital did end up being two and a half weeks. A day before bringing the girls home, Sam and I moved onto the ward and slept in a room there to get used to caring for the girls ourselves at night time. That was an experience in itself but was a helpful in between, as we got to prepare to take them home whilst still having the doctors’ and nurses’ support.
I have to admit that the closer we got to taking them home, the more nervous I got about it! We would be sent out alone with no nurses to help with feeds or changing nappies, no one to ask questions of, and no one to take over their care. Of course, it was still COVID time so we also couldn’t rely on family support. Our family couldn’t meet the girls until they were about a month or two old. We were truly on our own! (We weren’t, we had our faithful Father and a wonderful college community who kept us fed and well-stocked in nappies).



Thanks for joining me on this journey, it’s been wonderful and cathartic to look through my journals and photos from that time. It’s hard to believe those tiny babies are the same little girls currently hurtling around our living room. They are resilient, beautiful, and strong and we thank God that he blessed us with them, as crazy as they are. I hope you have found reading these posts eye-opening and interesting. If you ever are, or ever know, a NICU parent, I hope this post in particular is a helpful insight into what it’s like.